Only a doctor will be able to make a proper diagnosis to determine if surgery is necessary and/or recommended for your bursa. An MRI or x-ray may be necessary for an accurate diagnosis. An x-ray will show if the problem could be bone related, and an MRI produces an image of the muscles, tendons, bursae and ligaments that may be damaged or displaced. As you may know, bursitis and tendonitis occur very commonly together, and if there is both tendon and bursa damage, the MRI results will reflect this. MRI results are important as both surgery and the type of surgery undertaken will depend on whether there is only tendon damage or if there is bursa, ligament and/or muscle damage as well.
If all conservative treatment methods have been explored and your symptoms (pain as well as limited use for daily activities) persists, then you will be considered a candidate for surgery. You and your doctor may decide to move forward and have you undergo surgery, which will trigger the next chapter of your injury recovery journey. Your post surgery rehabilitation efforts will have an important impact on how soon you can return to living and enjoying your normal daily life.
The surgery that is selected for your injury will depend on the level of your pain and the amount of damage your doctor suspects there may be to your tendon(s) and secondary soft tissue (muscles, ligaments, bursae). Much of this damage will be determined through the use of physical exams, x-rays and MRI results. The length of time you have waited to have surgery will also be a factor that determines what type of surgery is needed.
With acute (recent) tearing, the separation in your muscle or tendon is likely to be very minimal. If you have an acute tear you may qualify for less invasive surgery (such as a arthroscopic, open surgery or an mini-open procedure). Surgeons will always choose a shorter, less invasive procedure if it's possible to do so. Most surgeons know that a less complicated procedure will cause less trauma to soft tissue in the area and increase your odds of a much quicker rate of recovery after the surgery.
If you're suffering from an acute muscle injury and surgery is needed your surgeon will most likely have you wait up to 72 hours before they'll start the repair to the muscle tissue. This gives your body time for the injury to settle down.
Muscles begin to atrophy (waste away) only after a few days of disuse. As time passes the muscle fibers shrink and the muscle loses strength and the (tissue) begin to die inside the muscle. (source: American Academy of Orthopedic Surgeons)
If scar tissue is present then a more complicated procedure may be needed to clean out the presence of any scar tissue for optimal healing after the surgery. The tissue that has ruptured may need to be retrieved from inside your other tissue back to the original attachment point. Your surgeon may make a larger incision into your skin so they're able to retrieve this tissue.
An injury that's 4 to 6 weeks old is considered a chronic rupture. When you have a chronic muscle or tendon rupture, the tear continues to separate further. A chronic rupture requires a difficult, drastic surgery - often times there may be a transfer of tissue needed to complete the surgery and a lengthy recovery period.
For most soft tissue injuries, arthroscopic surgery is the preferred procedure as it is minimally invasive and patients usually recover at a much faster rate. This type of surgery will provide the surgeon with first hand insight into the nature of the injury and possibly limit the amount of soft tissue damage from surgery, helping promote a more effective recovery. Some cases however, will require open surgery as the scope of arthroscopic surgery is limited in comparison to full exposure of the tendon or muscle in open surgery. If you undergo an open surgery, you should anticipate a much longer time for rehabilitation efforts.
As with any surgery there are risks to every procedure depending on a lot of factors, including your age, the severity of your injury and your level of health going into the procedure. It's always best to discuss all possible risks and complications with your doctor before the procedure. It's important to be aware of the risks you may face with any procedure intended to fix or relieve pain from your tendon injury.
Open surgery is considered the traditional surgery and nowadays is typically used when:
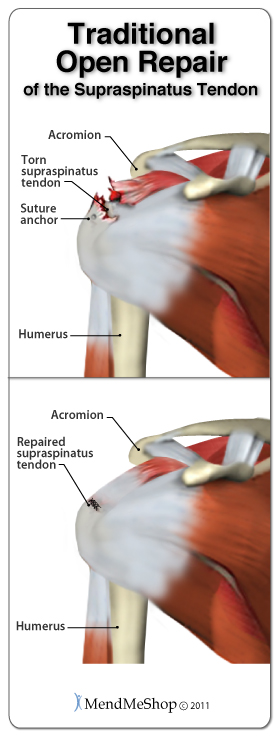
During an open procedure, typically one long incision is made in the area of your injury. An open incision this large provides enough room for the surgeon to prepare your soft tissue for repairing which could mean shaving down of bone spurs, removal of bone chips, removing frayed tendon/muscle pieces - basically cleaning up the area. Once cleanup is complete, the surgeon is freely able to grab the severed ends (in cases of full tears) and sew the tendon back together, typically using non-absorbable sutures to ensure the repair is as strong as possible. A small screw/anchor is used to reattach the tendon back to the bone if the it has been ruptured completely. Surgeons often use a strong nylon or polyester material to bring the edges of your torn tendon together. Sutures need to be very strong when dealing with tendons as the forces they deal with are extreme. Open surgery is used mostly in the hip, knee and shoulders.

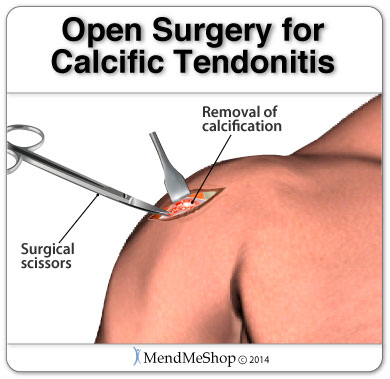
This surgical technique is done during open tendon surgery. To perform a debulking or debridement the surgeon will cut away any damaged/inflamed tissue and scrape down any calcium deposits (bone spurs) that have grown on bone. Scar tissue may be removed from the tendon fibers, tendon sheath surrounding the tissue or from both surfaces.
Debulking or debridement of the tendon is used as a last resort, if all methods of conservative treatment options have been exhausted, in chronic tendon conditions.
This procedure is typically used for conditions such as Tendocalcaneal bursitis, Achilles Tendinitis, Achilles (mid-point or insertional) Tendonitis and in some cases when the tendon has ruptured as well.
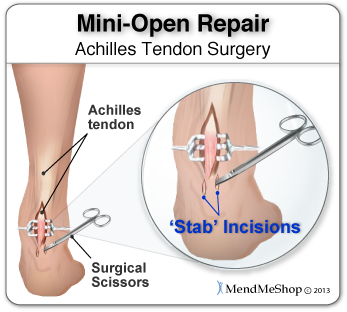
Depending on the area of your tendon injury, this procedure usually entails the the surgeon making one long incision in the skin and/or smaller vertical incisions as well. These smaller vertical incisions are made with a pair of surgical scissors and are commonly referred to as "stab incisions".
Once the incisions are opened up, the surgeon will place precise sutures in the tendon tissue as described above with the locking loop in non-absorbable stitches to strengthen the damaged tendon tissue. This suturing technique reduces the amount of scar tissue on the tendon after surgery and provides better surface healing of the skin. Unlike the traditional method of an open surgery, this procedure has less risks and complications involved. To learn about all risks you may face be sure to speak to your doctor.
Your surgeon may choose to perform your surgery arthroscopically if your damaged tendon is accessible through 2 to 4 keyhole incisions. This procedure is done using 2 to 4 small keyhole incisions approximately 4 to 5 mm in length; a thin tube containing a camera and light are inserted through an incision near the joint. Additional surgical tools required to remove/fix your tendon will be inserted into the other keyhole incisions. This type of surgery will provide the surgeon with first hand look into the nature of the injury without the additional damage that is typically encountered with open surgery.
Arthroscopic surgery is intended to be a minimally invasive procedure as it will help limit the amount of tissue damage from surgery, helping promote a more effective recovery. Your surgeon will perform surgery with the goal to have you on the road to recovery faster. Rehabilitation from this type surgery will depend on your healing ability, rest, your diet, tissue damage, and other procedures done during the surgery.
During this procedure the surgeon will make 3 to 4 incisions (approx. 2.5 cm long) in the skin. Small forceps are used to free the soft tissue casing around your damaged tendon to make room for the surgeon to stitch/suture any tears.
Instead of making several 2.5 cm incisions for this procedure, they will use a surgical needle to repeatedly stab your tight and constricted tendon. These "stab incisions" will allow the surgeon to lengthen your tendon without seeing the actual tissue. This type of tendon surgery has been very successful in providing range of motion. In most cases the tendon in question has had open surgery with unsuccessful results and a build-up of scar tissue has further tightened the tissue.
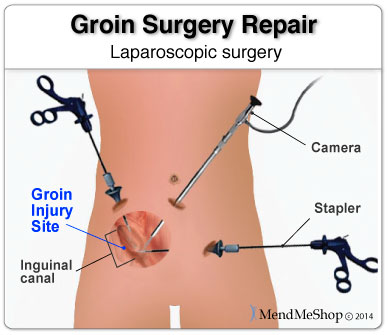
Laparoscopic surgery is basically an arthroscopic type of surgery that if performed on the abdomen/groin. During this procedure the surgeon will make 3 small holes in your abdomen. Small incisions (about 1/4 inch each) are made below the belly button and a small, fiber-optic camera (laparoscope) is inserted to give the surgeon a first-hand look at the tissue that needs to be repaired.
The surgeon will then repair your groin injury with a few sutures or a mesh screen that's attached with surgical staples. Since this procedure only uses a few small incisions you will generally have a brief recovery period using conservative treatment methods (heat, ice) and get back to your normal activities within 4 to 6 weeks. This is normally an outpatient procedure; which means that you'll go under general anesthesia and get sent home the same day as your surgery. Unlike the traditional method of an open surgery, this procedure has less risks and complications involved.
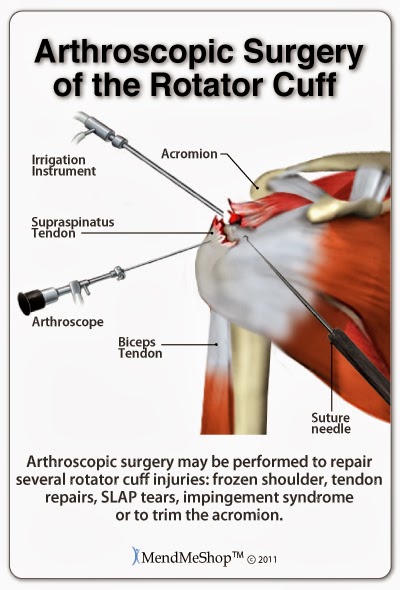
The surgery that your surgeon will recommend for you will depend on the level of your pain, the type of injury to the shoulder, and the amount of damage assessed via information gained from your physical exams, x-rays and MRI results.
It is always highly recommended that anyone considering surgery always have a clear understanding of the risks as well as the benefits of elective surgery. In addition, one should also be aware of the success rate of the particular surgery in question combined with the post-surgical recommendations that will typically have an impact on your chances of success. As an example, in nearly all cases of rotator cuff repair surgery (in both arthroscopic and open), immediate postoperative physio (stretching, exercise) is initiated generally lasting from 12 to 16 weeks. Your surgeon should provide a treatment plan to help you regain normal use of your shoulder as soon as possible.
The rotator cuff surgery to repair a torn rotator cuff muscle or tendon usually involves one or more of the following surgical goals:
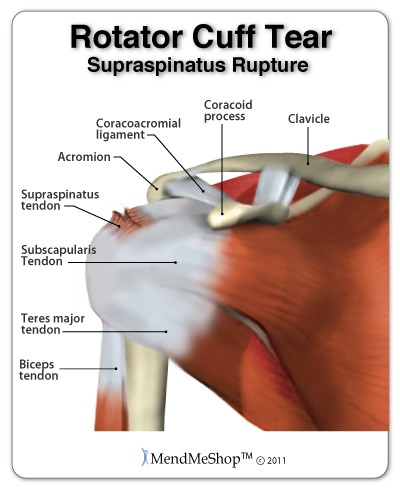
Common conditions treated with shoulder surgery may include Calcific Tendonitis, Rotator Cuff (Supraspinatus Tendinitis) and Bicep Tendinitis
Shoulder arthroscopic surgery generally means that the surgeon will make tiny incisions around your shoulder joint and insert a pencil-thin camera with a small lens and lighting system. These images will then be transmitted to a TV monitor, which allow the surgeon to make a diagnosis and/or perform the repairs needed in the rotator cuff.
Impingement syndrome or a partial thickness Rotator Cuff tear are best treated by this type of surgical repair. They may require a debridement and/or shaving or removal of bone spurs and fragments that can catch when your arm is rotated. At the end of surgery, your incisions are closed, and a dressing is applied. As arthroscopic surgery is minimally invasive and patients usually recover at a much faster rate.
This type of surgery is often the first choice of most surgeons. If you have a complex or full thickness rotator cuff tear, the surgeon will use sutures (stitches and/or metal or plastic anchors that hold the tissue together after they have been severed) to help attach the tendon back to the tissue or bone.
Open repair surgery is also used when additional reconstruction is required, such as a tendon transfer and/or shoulder replacement.
There are always some risks with any surgery, which may include possible infection, allergic reaction to medications, and damage to surrounding nerves or blood vessels. Surgery always will lead you to have more tenderness, pain, stiffness and weakness after surgery, but with proper rehabilitation these should diminish.
Surgery is often recommended for younger individuals, people who continuously use their shoulder for work, athletes, or when non-surgical treatments are not effective. Although surgery is often successful at repairing any damage and/or relieving pain, it does not necessarily return strength to your shoulder. That's why a strong commitment to rehabilitation is essential.
After the surgery is done, you can expect to undergo recovery and rehabilitation efforts for several months. Range of motion movement is encouraged early, with restricted motion within days after surgery. This is an important step as your body heals scar tissue is forming.
If you have been suffering from a chronic condition your surgery will be more involved and your recovery time may be longer than normal. Shoulder strength and range of motion return, usually after after 6 to 8 weeks with regular PT sessions included as part of your shoulder recovery.
Depending on your job (and whether your occupation has caused your condition), you may be able to return back to work within a few months. Overall healing of your shoulder after surgery may take upwards of 4 to 6 months, which means you may not be able to return to sports or heavy use of your arm for some time.
Posterior Tibial Tendonitis, Peroneal Tendonitis, Sesamoiditis and any type of toe deformities - typically all require open surgery to remove and/or repair the damaged tissue. You may be placed in a cast or splint and use crutches for 4 to 12 weeks. This will depend on how chronic your condition was before you have surgery. Complete recovery may take 6 months to one full year before you may gain complete range of motion in your foot or ankle after surgery.
Traditional open surgery involves the surgeon making a 4cm open incision on the side of your foot. The fascia will be partially cut across the surface of the ligament - close to where it attaches at the heel bone. A surgical retractor is used to further widened 'gap' of the incision. The surgeon may also address any calcium deposits and/or bone spurs during the operation.
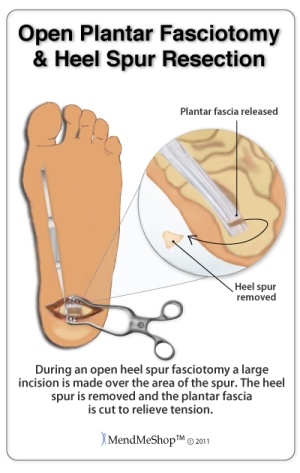
It should be noted that the plantar fascia is not fully detached from the heel bone during this procedure - only a portion of the ligament is detached. Once the first cut of the ligament is done, the surgeon will use his/her judgement to determine if the fascia is still too 'tight' and continue on in this manner. Another small 2cm incision is typically made just at the base of the ball of the foot, further exposing the fascia. With the fascia exposed more, cuts are placed in the ligament and the surgeon will manually push your foot in an upward motion (put strain on the fascia) to ensure the 'release' of the tissue. Once complete, the surgeon will apply surgical sutures to close the skin wound(s); during recovery you may be fitted with a non-weight-bearing cast or brace for 2 to 3 weeks allowing the tissue to heal
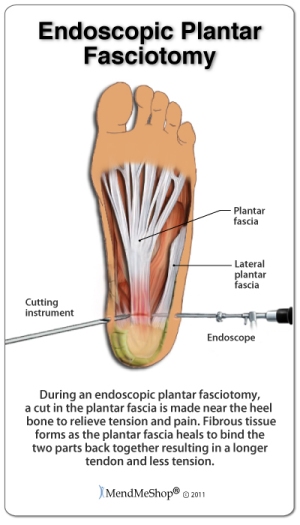
Newer tools and techniques mean endoscopic surgery has become the 'gold standard' for plantar release (fasciotomy). Normally, an endoscopic release is a day surgery that only requires a local anesthesia.
During this type of surgery, the surgeon will use one or two 1 cm small incisions on either side of the heel below the ankle bone. A small camera and scalpel are inserted and a portion of the plantar fascia is cut from the heel bone. (No removal of any calcium deposits and/or bone spurs are done in this surgery.) Much like a tradition fasciotomy, the surgery will then flex your foot in an upward motion to ensure the 'release' of the fascia tissue. The skin is then sutured close and in most cases you are sent home. In many cases you can begin limited weight-bearing activity immediately and wearing normal shoes again as soon as you are comfortable. Most people can return to normal activities in 3 to 6 weeks.
Unlike the traditional method of an open surgery, this procedure has less risks and complications involved. To learn about all risks you may face be sure to speak to your doctor.
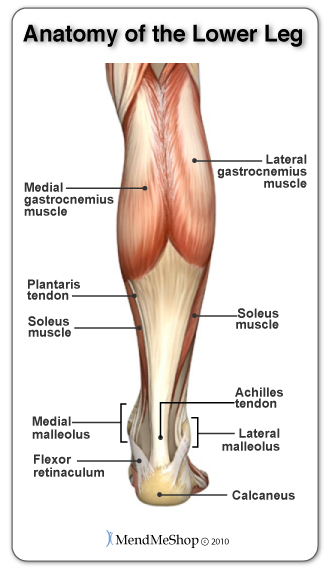
A Gastrocnemius Recession is the probable surgery performed if you are experiencing limitied range of motion when flexing your feet upward (putting strain on the calf muscle) despite your physician or PT prescribing a long period of calf stretches. This type of surgery is performed to lengthen the calf muscles (gastrocnemius) - thus allowing your foot a larger upward range of motion. When the calf muscles become tight, increased stress is placed on the plantar fascia and as such plantar fasciitis is often a secondary condition with the causal factor being a tight calf muscle.
During the gastrocnemius recession surgery, a 4-7 cm incision is made on the back inside part of the lower leg. Controlled depth incisions are made in the Medial gastrocnemius muscle (or complete release) and plantaris tendon. A surgical retractor is used to further widen the 'gap' of the incisions. The surgeon will move the foot and ankle to see the results in the new range of motion and from there determine if more incisions are needed to 'release' the tissue. The skin is then sutured close and you are placed in a right angle cast, brace or splint for the first two weeks. After this you will most likely transition to a walking boot. It is important to strengthen the calf since you will lose strength in the short term and your Physicial Therapist will most likely focus on strengthening and range of motion. By the 6-8 week mark, you can usually walk normally though it may take 8-12 months to regain 90-95% of the original calf strength.
Neurolysis involves cutting the nerve sheath of the abductor digiti minimi muscle and breaking up adhesions (scar tissue) to free the nerve and relieve the pressure and pain from inflammation. Radio frequency, heat, or chemical injection, have also been used.
Most of the surgeries for plantar fasciitis require a recovery time of approximately 1.5 months. Sometimes a removable cast will be used to support and immobilize the foot. Occasionally crutches or a cane will be used to minimize weight bearing.
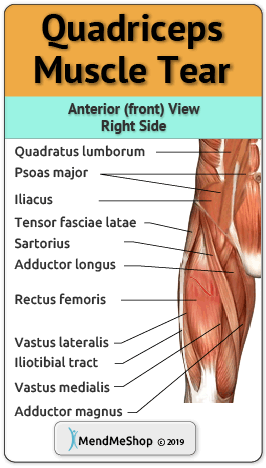
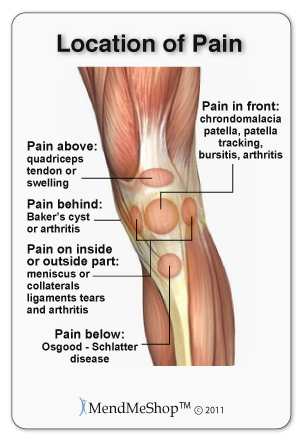
Common tendon conditions treated with knee surgery may include Pes Anserine Tendinitis, Quadriceps Tendonitis and Hamstring Tendonitis.
The type of surgery you will have depends on the type of knee injury you're suffering from. The longer you've waited to have surgery will also be a factor that determines the type of sugery that's needed.
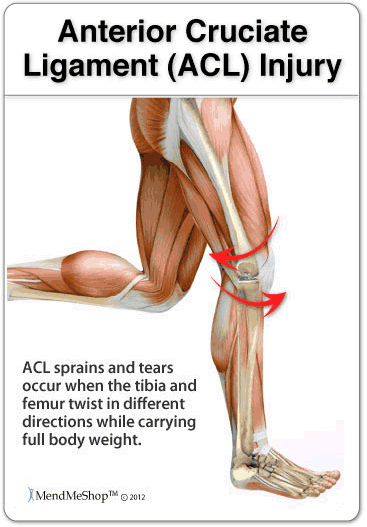
With acute (recent) tearing the stretch or tear in your tendon/ligament or the damage to your bursa/meniscus may be minimal. If you have an acute tear that is relatively small you may qualify for less invasive surgery (like an arthroscopic procedure). Surgeons will always choose a shorter, less invasive procedure if it's possible to do so. Most surgeons know that a less complicated procedure will have less trauma to your knee and a much quicker rate of recovery after the surgery.
If you're suffering from a chronic knee injury or tissue tear that's been going on for a while (from overuse/repetitive movement) or has been damaged due to aging of your soft tissue, then you may have less options available for surgery. A repair of soft tissue in the knee, for example, is usually only ever performed for newer (acute) tissue tears where it is possible for the tissue to heal back together. If you have a chronic knee injury there may be more fraying to your ligament or tendon tissue. If you suffer from chronic knee bursitis, it's likely that you also have another soft tissue knee injury (like tendonitis or a torn ligament) that keeps causing your bursitis to recur. In either case arthroscopic surgery may be enough to fix your knee but the amount of tissue that can be repaired will depend on how worn away/frayed (degenerative) your tissue damage is.
Your age will also be a factor. Surgery is generally used more often for younger patients requiring a repair to a tendon or ligament tear. Conservative treatment methods and PT are recommended (instead of surgery) for older patients suffering from the same type of injury. (reference: 1)
Even if surgery is required to treat your knee injury, your surgeon may still recommend PT before the procedure. This is sometimes recommended so you may strengthen your quadriceps and hamstring muscles. This is done to help with your post-surgery recovery.

There are 2 main types of surgery: knee arthroscopy and open knee surgery. Arthroscopy is by far the most common procedure used when performing a knee surgery. It's a doctor or surgeon's preference to perform an arthroscopy whenever possible, because it's the least invasive surgical procedure and usually has the quickest form of rehabilitation afterward.
Whether you'll qualify for an arthroscopy depends on the severity and type of injury that you have. In many cases, arthroscopy is also used to examine an injury for diagnosis, because this procedure is done with a thin tube containing a camera and light inserted through an incision near the knee joint. This type of surgery will provide the surgeon with a direct look into your injury and help to limit the amount of additional damage from surgery. During this surgery your doctor will only make 2 to 3 keyhole incisions (less than 1 inch in length) to insert the thin tube with the camera, an irrigation instrument and any surgical tools they will need to fix your knee. There will be minimal surface damage to your knee and in some cases; the tiny incisions won't even require stitches to heal.
If you suffer from a more severe knee injury you may need to have an open knee surgery to give the surgeon a better view of your injury and more room to move the surgical tools around if your injury is complicated to fix.
When researching your options for surgery you may find more information available about arthroscopic surgery. This is because arthroscopy is considered to be the gold standard for knee surgery, meaning that many surgeons prefer to perform an arthroscopy to minimize the how invasive your surgery is. Most doctors and surgeons will automatically consider you for arthroscopy whenever possible to provide you with the fastest rehabilitation and recovery option after surgery.
If, however, you have a severe injury - like a full tissue tear, an open wound from a traumatic event or an accident, bone damage, displacement or fracture, or require a full knee replacement - then you will probably have to undergo an open knee surgery.
In an open knee surgery your incision could be 6 to 10 inches in length - or longer if you already have an open wound. During the surgery, instead of making a few keyhole incisions like in the arthroscopy, your surgeon will open up your knee to see the inside joint. This means your surgeon will cut through your skin and the muscle underneath to see your injury. Open knee surgery will probably leave a scar on your knee - the possibility of a scar being yet another reason why surgeons will avoid open surgery wherever possible.
Knee Arthroscopy is considered an outpatient surgery (most of the time you can leave the hospital the same day as your surgery) but this is not the case for open surgery. Open surgery is considered an inpatient surgery which means you'll almost certainly have to stay overnight or maybe even longer.
During the first 24 to 72 hours after surgery your knee will be tender, swollen and very painful. Your knee may be weak and unstable, and depending on your surgery, you may have to weara knee brace or use crutches for a few weeks. One of the things to keep in mind when recovering from knee surgery is the importance of resting in the beginning, but getting active and going through rehabilitation when it's needed. When you're recovering from surgery and using tools to keep weight off of your knee (like a knee brace or crutches) then your knee and the surrounding muscles aren't as active as they once were.
Recovery time will depend on the amount of damage to the tendon tissue before surgery and if it is an acute injury or chronic (old, long lasting injury). Recovery time from knee tendonitis surgery is 2 to 4 weeks and in this timespan your leg can usually bear about 50% of your body weight. After 4 to 6 weeks, your leg should be able to handle your full body weight. Reaching full complete recovery may take 6 to 12 months.
If you fail to deal with proper rehabilitation of your knee after surgery, muscle loss (atrophy) will occur in your leg. The soft tissue and cartilage in your knee joint may start to wear away (a process called degeneration). There is always a risk of re-injuring your weakend knee after a surgical procedure has been done so be careful.

Hip arthroscopy can be a minimally invasive surgical procedure that is used to diagnose and/or treat hip conditions. If a doctor is unable to make a diagnosis following a physical exam, x-ray, and/or MRI, an arthroscopy may be performed to get a better look inside the hip joint so a diagnosis can be made.
Depending on the severity and type of injury and the age and activity level of the patient, hip arthroscopic surgery may be required for repair if nonsurgical treatments have not shown improvement in pain, range of motion and other symptoms.
A hip arthroscopy is usually performed with the patient under general anaesthetic. During surgery, tiny incisions (1/4" - 1/3") are made to insert the surgical instruments and a small arthroscopic camera that provides an internal view of the location of the surgery.
If you're suffering from a secondary condition along with tendonitis such as bursitis, your surgeon may need to add 1 to 2 more incisions for additional soft tissue repair. Your tendon may end up being much looser than before you had surgery. Generally, the surgeon wants to make sure your greater hip tendon tissue isn't rubbing on the surface of the other tissue in your hip and your don't continue to suffer from this condition
Arthroscopic surgery is also used to treat knees, elbows and pretty much any other joint... however, the hip is a deeper joint and it can be difficult to insert the instruments and camera at the proper location. As a result, the hip joint may be distracted (opened up) by traction so space is created and the instruments can be used without damaging the labrum, cartilage and other soft tissue.
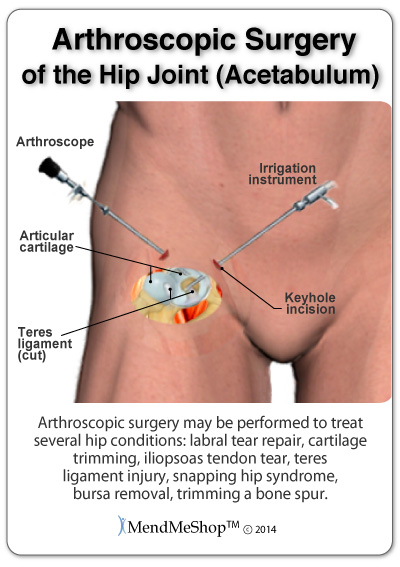
Common conditions treated with hip surgery may include Gluteus Medius Tendonitis, Hip Flexor Tendonitis (Iliopsoas & Iliacus Tendonitis), Iliotibial Band (IT Band) Tendonitis / Syndrome.
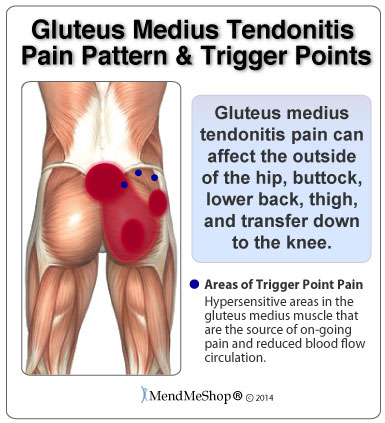
Post-operative recovery from hip tendonitis surgery will mean that you'll most likely be on crutches for 2 to 4 weeks - the duration will typically depend on what was done during the surgery but also whether the surgery was open surgery or arthroscopic. You'll also need to wear a brace for a couple of weeks to protect the delicate tissues in your hip and prevent extreme movement. The brace will need to be worn over your clothing during weight bearing activities while still using your crutches. You may also need to wear the brace while you sleep for the first week after surgery.
You'll have to attend a PT clinic quite a few times a week during your post-surgery recovery. It may even take several months. You'll be encouraged to move around as soon as possible, but with care placed on protecting your hip and the tissues as they heal.
"Traditionally, the standard procedure for lateral epicondylitis has been an open release"
Reference: Nirschl RP, Pettrone FA, 1979. "Tennis elbow. The surgical treatment of lateral epicondylitis." J Bone Joint Surg Am 61 (6A): 832-9
"Open release is simple and reproducible with excellent results and still considered the 'gold standard'. Open release has good long-term results. A study by Dunn showed that 84% of patients had good to excellent results and 93% returned to sports at minimum 10-year follow-up. Nirschl and Petrone also reported excellent results in 75% of patients with open release."
Open vs. Arthroscopic Treatment of Lateral Epicondylitis - OrthopaedicsOne Viewpoints - OrthopaedicsOne "Open Vs. Arthroscopic Treatment Of Lateral Epicondylitis - Orthopaedicsone Viewpoints - Orthopaedicsone." Orthopaedicsone.com. N. p., 2018. Web. 8 May 2018.
The elbow joint is one of the most flexible joints yet the skin of the elbow is thin. High flexibility of the elbow means soft tissue is stretched significantly in this joint yet lack of blood flow makes damage to elbow soft tissue very hard to heal. Arthroscopic surgery or percutaneous tenotomy are the preferred procedures as they are minimally invasive and patients usually recover at a much faster rate. Some cases however, will require open surgery as the scope of arthroscopic surgery is limited in comparison to full exposure of the elbow in open surgery. If you undergo an open surgery for your Elbow Tendonitis, you should anticipate a much longer time for rehabilitation efforts.
Depending on your job (and whether your occupation has contributed to causing your condition), you may be able to return back to work between 6 to 12 weeks after the surgery. Overall healing of your elbow after surgery may take upwards of 6 to 12 months, which means you may not be able to return to sports or using your arm to do heavy activities, until a year has passed after your surgery.
The most common surgery used to treat Tennis Elbow is Open Release Surgery. There are two different techniques that can be used, Traditional Open Release and Open Release with Drilling; both been successful in treating Tennis Elbow.
Open Release is performed through a 2.5 - 7 cm incision created in the skin on the outside of the elbow above your epicondyle. This incision exposes the ECRB (exstensor capis radialis brevis ) forearm muscle beneath the skin. Another incision in the muscle gives the surgeon access to the tendon and its attachment to the lateral epicondyle bone. The surgeon will either remove any damaged weakened tissue, or repair tears to the tendon tissue. Your surgeon may be partially or even completely cut your tendon away from the lateral epicondyle. This allows the forearm muscle to relax.
Scar tissue that has built up through repeated injury and overuse is removed through a process called Debridement. During the removal of scar tissue and normal wear and tear, the elbow can become rough. The surgeon will abrade the bone of your elbow. This smoothes out the roughness of your elbow and removes any hardened tissues.
A technique called decortication can be used at this point. With this procedure, several 2 mm holes are drilled into the bone to stimulate blood flow to the area.
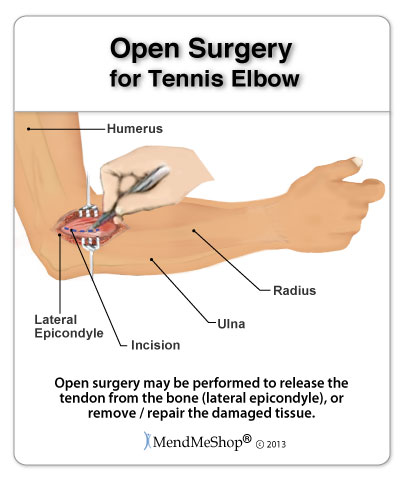
Bone and cartilage debris is taken away and sutures are installed using anchors to reattach your tendon to your bone. The surgeon will use dissolving stitches to seal the first cut made in your skin. Your arm will be placed in a splint or cast to keep from moving your elbow until your doctor says you are ready to begin light movements.

A 2001 study published in the British Medical Journal evaluated open and arthroscopic release surgeries. While both were found to be successful in the long term, drilling was no more effective in treating Tennis Elbow than traditional open release surgery. In fact, patients who underwent the drilling procedure were found to have more pain, stiffness, and bleeding of the wound than non-drilling patients during recovery.
Arthroscopy for Tennis Elbow involves creating very small incisions in your skin at and around the epicondyle. These incisions act as entry points for thin tubular instruments to be inserted into your elbow. One of these tools is a small, high powered camera that uses a fiber optic lense to record the inside of your elbow. Fluid is injected into your joint so the camera can give a clearer image and the surgeon has a better view of your elbow during the procedure. The images captured by the lense are sent to a television screen so that the surgeon has a magnified view of the inside of your elbow.
The surgeon will inspect your elbow joint and see if there are any other issues, such as arthritis. Once your elbow has been fully checked out, another incision is made, so that tools for removing tissue and tendon repair can access your elbow. Using the guidance of the imaging on the television screen, the surgeon uses a sharp tool to remove inflamed and damaged tissue.
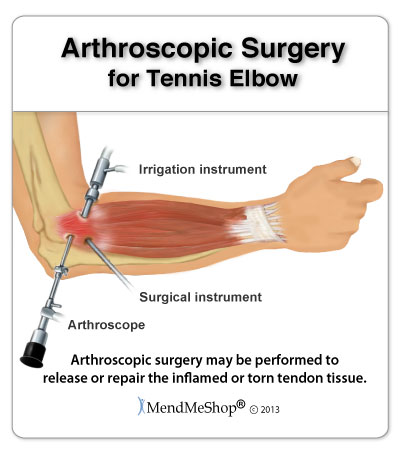
Another tool cuts away part, or all of, the tendon depending on the amount of damage. Once the scar tissue and hardened joint tissues are removed, the epicondyle is smoothed. Anchors are drilled into the bone to help sutures reattach the tendon to the bone. Once this is done, the tools are removed and the incision points are stitched shut. Your arm is splinted to prevent movement.
While both Open Release and Arthroscopic surgeries are 80 - 90% effective, arthroscopic surgeries have the added benefit of:
The Journal of Shoulder and Elbow Surgery, showed 91 - 98% success rate for full symptom relief of Tennis Elbow after arthroscopic surgery. Since arthroscopy can not only repair known injuries but also identify other conditions, this study concludes that arthroscopic surgery could be more beneficial than other surgical options available for Tennis Elbow.
Percutaneous Tenotomy is a new, alternative form of surgery for Tennis Elbow. This procedure was recently introduced in the early 2000's. Studies are still being conducted to verify the effectiveness of percutaneous tenotomy, and all have shown positive results. This procedure does not require an anaesthetic, like in Open and Arthroscopic procedures. The only entry points into your elbow are made via a hypodermic needle.
This procedure uses sonographic images, similar to those used in prenatal care, to view the unborn child of a pregnant mother. These images, created using imaging ultrasound waves, help guide the surgeon, while repeatedly penetrating the joint tissues of the elbow with the tip of the needle. The surgeon can feel when the tissues have become softer. Once hardened tissue has been broken up to allow access to the bone, the surgeon uses the head of the needle to smooth out the epicondyle. Removing damaged tissue without having to cut the tendon is one of the major benefits of percutaneous tenotomy.
The hypodermic needle is removed when the sonographic images show that all of the hardened tissue has been broken up and the epicondyle is smooth. At this point your elbow will be injected with a shot of corticosteroid. This step is under review and future percutaneous surgeries may not require the coticosteoid injection at all. Medical tape is placed over the incisions and there is no need for stitches
Because this procedure does not require an anaesthetic, it can be performed in a clinic or at a doctors office. Directly after the 20 minute surgery is completed, the physician will help you to gently move your arm. Unlike open and arthroscopic surgeries, percutaneous surgery does not require you to wear a splint to keep your arm from moving. In fact without large incisions or sutures, the risk for infection is greatly reduced.

According to an article published on December 2nd, 2012 in the online US National Library of Medicine, many individuals found immediate pain relief after the soft tissues were broken up. This is however, still a newer method of surgery, therefore we anticipate many more studies to follow, concerning the overall effectiveness of this procedure.
Product Advisors are available 9:00 am to 5:00 pm Eastern Standard Time Monday to Friday.
I want to learn more about Post-Surgery Recovery
I want to learn more about TShellz Wrap® Circulatory Boost
I want to learn more about Ice & Heat: Which Is Better For Treatment?
I want to learn more about Tendonitis Treatments
I want to learn more about Tendonitis Surgery
During your recovery, you will probably have to modify and/or eliminate any activities that cause pain or discomfort at the location of your soft tissue injury until the pain and inflammation settle. The more diligent you are with your treatment and rehabilitation, the faster you will see successful results!
Please be aware that this information is neither intended nor implied to be a substitute for professional medical advice. CALL YOUR HEALTHCARE PROVIDER IMMEDIATELY IF YOU THINK YOU MAY HAVE A MEDICAL EMERGENCY. Always seek the advice of your physician or other qualified health provider before using any of our outstanding products to make sure they are right for you and your condition or if you have any questions regarding a medical condition. Always see your doctor for a proper diagnosis as there are often many injuries and conditions (some very serious) that could be the cause of your pain.
© 2025 In.Genu Design Group, Inc. Contact Us