Knee pain is a very common problem and there could be a variety of causal factors to your injury. Knowing that the knees handle a lot of force and have a large number of muscles, ligaements and tendons attached, It's important to have a correct diagnosis of the cause of your symptoms. This way the right treatment can be used to solve the condition and treat your pain.
The knee joint is the largest joint in the human body and consists of 3 bones: (1) the thighbone (femur), (2) the shinbone (tibia), and (3) the kneecap (patella). In mechanical terms, it is considered a "modified hinge joint" and permits flexion and extension while also permitting slight internal and external rotation (twisting).
There are many muscles that attach in the knee joint area - 6 extensors (mostly hamstring muscles), 7 flexors (quadriceps, tibialis anterior, popliteus) and the gracilis muscle. Further to this, there are 4 major knee ligaments - the most widely known being the Anterior Cruciate Ligament (ACL). The other 3 ligaments in the knee are the Posterior Cruciate Ligament (PCL), the Medial Collateral Ligament (MCL) and the Lateral Collateral Ligament (LCL). With so many connections of tissue to bones in the knee combined with the fact that the knee handles our body weight on a constant basis it's easy to see why knee pain is so common.

Soft tissue such as tendons, ligaments and muscles, have a very important role in our daily movement of the knee and legs. This large hinge joint is placed under stress regularly. The tissue is pushed, pulled and twisted even while walking, which can lead to tiny tears in the connective tissue from muscle to the tendon. Acute injuries in the knee can often cause tendon separation from bone and ligament tears - an ACL tear is a very common injury.
Tendinitis in the knee happens in older adults due to degeneration of tissue as we age (repetitive, chronic injuries). Over time the tendons in the knee will wear down resulting in something called degeneration. This is where the fibers in your tendons will become more weak - it's just a natural process that happens as we age. Tendinitis in the knee also happens to younger people though it is typically due to a specific incident or accident - often occuring during a sporting event (football, soccer, hockey, basketball, etc).
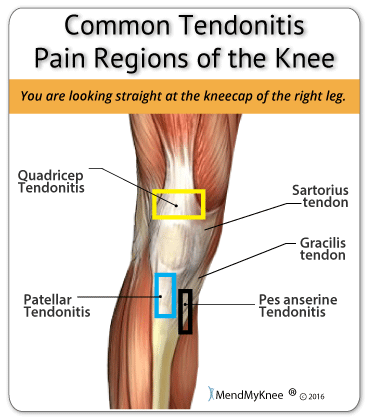
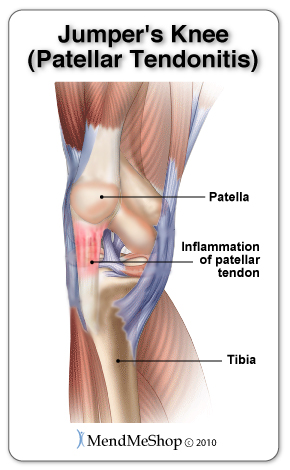
Tendons in the knee usually get injured from athletic or sporting activities like rugby, football, volleyball, or any activity involving running and jumping. Individuals with arthritis or osteoarthritis in their knee may also experience knee tendonitis due to the degeneration of bone and tissue in their knee joint. The most common type of knee tendonitis is patellar tendonitis, also sometimes referred to as 'jumper's knee'. If you have knee tendonitis some of the symptoms you'll experience are pain, swelling and inflammation around the injured area. The severity of your pain depends on the amount of damage that's been done to your tendon. Some other common forms of knee tendonitis include quadriceps tendonitis, pes anserine tendonitis, hamstring tendonitis and popliteus tendonitis.
Knee tendonitis can occur in any of the tendons that surround the knee joint. If you have knee tendonitis some of the symptoms you'll experience are pain, swelling and inflammation around the injured area. The severity of your pain depends on the amount of damage that's been done to your tendon. The most common forms of knee tendonitis are:
Pain in the section of the knee between your knee cap and your shinbone. The patellar tendon is important role with the movement of you leg. The patellar tendon helps your muscles extend your knee so that you can kick a ball, run uphill and jump up in the air. Tendonitis is a condition that is micro-tearing in the tendon tissue. When the knee is overworked or overstressed the damage to the soft tissue is done. More common in an aging athlete who is involves in "jumping" sports such as basketball, volleyball and jogging.
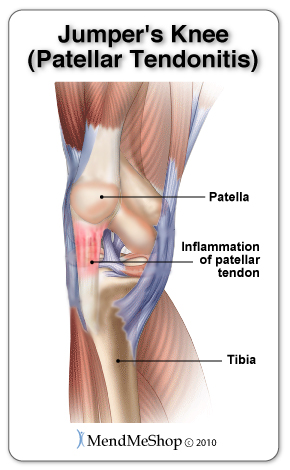
For more information about patellar tendonitis, click here.
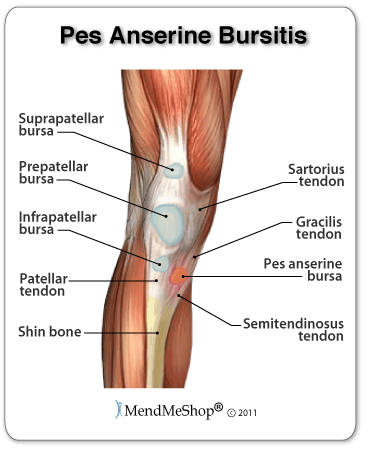
Pain in the knee on the inside of the knee just close to the kneecap. The Pes Anserine tendon has been overuse or overstressed and the tendon tissue has been damaged. The tendons connects muscles to bones, and the damage is small micro-tears on the tendon fibers. The cause is weak hamstring muscles, tight quadriceps muscles, poor sport techniques, issue with your feet rolling inward or outwards. Pes Anserine Tendinitis is a common injury with runners.
For more information about pes anserine tendinitis, click here.

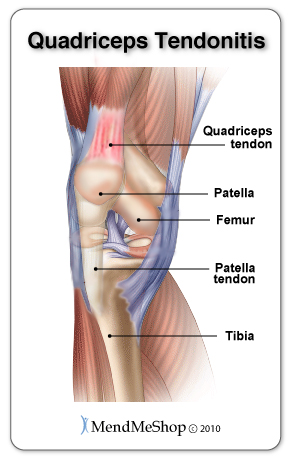
Pain in the area at the bottom of the thigh, just above the knee cap. The most noticeable pain is when you move your knee, the more you move the more tenderness develops in the area of the tendon attachment just above the kneecap. This condition is most common in an athlete who are involved in sports that require a lot of jumping such as basketball, volleyball and jogging, or in a sport that requires a lot of stopping and starting. The quadriceps tendon works with the muscles in the front of your thigh, they work together to straighten your leg.
For more information about quadricep tendinitis, click here.
Aching and stiffness which become more noticeable first thing in the morning. You may feel weak in the knee and swelling in the thigh and calf muscles. You may fell a gradual pain in the back of the knee when continues to get worse with activity. Sports that involve a lot of running and jumping or rapid changing of speed while running. This over use of the hamstring muscles damage the connective tissue in the tendon. The hamstring tendon is the soft tissue which connects the hamstring muscle to the outer side of the knee. Hamstring tendonitis is caused when the tendon becomes damage from overuse or excessive strain or force being placed on the tendon.
For more information about hamstrings, click here(aidyourhamstring.com).
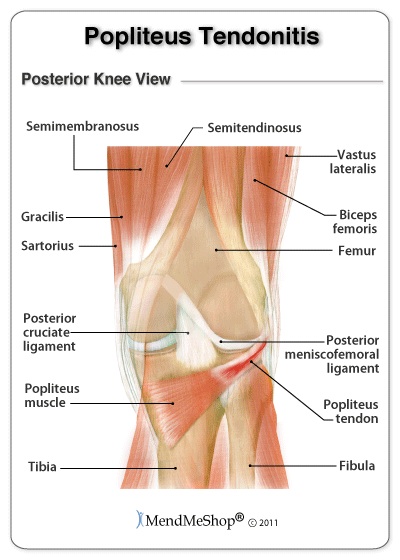
The general symptom of popliteus tendinitis is pain at the back of the knee in the fold of your leg. Walking downhill or extensive running will increase pain. Standing on a slightly bent knee or rotating the knee may increase your pain. For runners with a chronic condition they will have pain at the beginning of a run. The popliteus tendon, which connects the popliteus muscle to the thigh bone (femur) near the knee. The popliteus muscle/tendon helps you bend and rotate the knee.
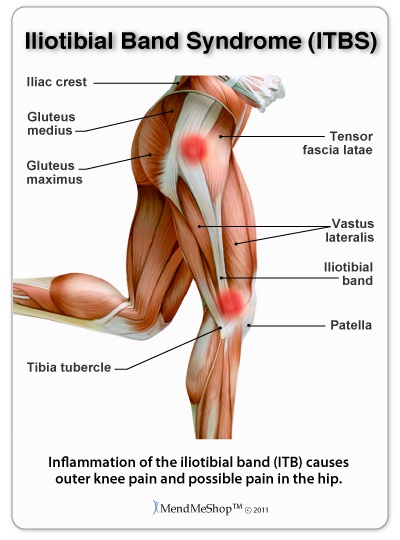
Pain on the outside the hip or the knee. The iliotibial band is a band of fibrous tissue that runs down the outside to the thigh from your hip to your knee. It provides stability to the hip and knee and its' job is to prevent the dislocation of the knee and hip joint. When the IT band becomes tight it rubs across the hip bone or the outside of the knee every time we move. This constant rubbing can cause degeneration (break-down) of the IT band tissue, or move the IT band over the hip bone. Pain normally disappears as you stretch out the hip and knee. The tissue becomes more flexible and pain improves with rest.
For more information about IT Band Tendinitis, click here.
There are 2 form of tendonitis, acute and chronic. Acute means that comes on suddenly, usually from a tendon strain or overloading it during exercise. Acute tendonitis refers to inflammation caused by damage via small micro-tears in the tendon fibers. Chronic means recurring, any form of tendonitis occurs over time and generally results from long term repetitive use of the quadriceps tendon.
With both types of tendinitis, scar tissue develops on the tendon as the tears begin to heal. This scar tissue mends the tears in an abnormal way leaving the tissue fibers weaker and more prone to further injury. In the case of chronic tendinitis, a build up of scar tissue over a long period of time will make the tendon and the entire knee joint more prone to re-injury.
Many back, spine, hip, foot and ankle problems can cause symptoms around the knee. You are also at greater risk of having knee problems if you are overweight. This is one of many reasons for visiting your doctor, as they can determine causal factors for your knee pain that can be easily overlooked by a layperson. Sometimes, one set of symptoms can result in multiple diagnoses.
The only way to know whether you have hip tendonitis for sure is through a diagnosis or consultation with your doctor. Physical examinations, magnetic resonance imaging (MRI), x-rays and other tests can help to determine if you suffer from hip tendonitis, or some other condition in your hip, back, hamstring, or buttock.
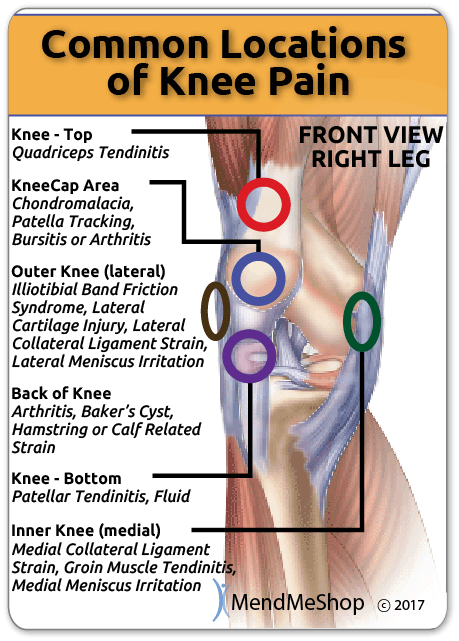
Understanding what is causing the pain is the first step in knowing how to treat your injury and stop the pain. The location of the pain in your knee can give you an idea of what may be causing your pain; however, a proper diagnosis from a doctor is important to ensure you are treating the right condition and to rule out any underlying factors that may go unnoticed.
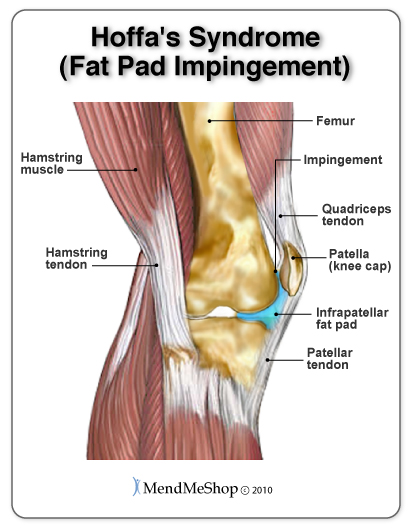
Occasionally other conditions may be associated with tendonitis including diabetes, gout, para-hypothyroidism. Other conditions which can be a cause of anterior knee pain are commonly confused with tendonitis. These conditions include synovial plicae, Chondromalacia, patello-femoral subluxation and hyper-pressure, fat pad impingement or Hoffa's syndrome and patello-femoral arthritis.
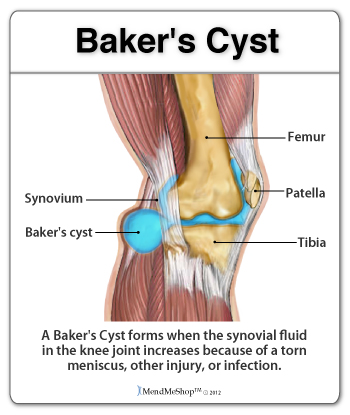
A ganglion cyst or synovial cyst can occur in any joint in the body. They appear under the skin as a lump or bump (non-cancerous) and may sometimes present no other symptoms. The cyst is basically a soft sac filled with a thick, clear fluid. It's still unknown why cysts form so close to a joint or tendon.
Cysts may or may not become painful (in a lot of cases they're harmless), will limit your activity and could possibly grow larger if you continue the activity that caused this injury in the first place. Usually cysts only become really painful if the cyst is pressing down on any nerves in the affected area. If this is the case, then you may suffer from pain, tingling, numbness or muscle weakness.
If you don't have a lot of pain then you may only need to treat the symptoms of your cyst and wait for the cyst to naturally go away on its' own. Cysts most commonly show up in the wrist, hand, ankle, feet and near other joints. A cyst that forms at the back of the knee is known as a baker's cyst.
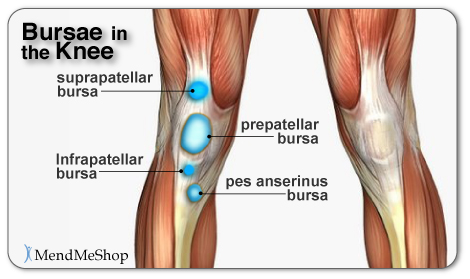
Bursae (plural for bursa) are flattened fluid-filled sacs that function as cushions between your bones and muscles (deep bursae) or bones and tendons (superficial bursae). They reduce friction and allow the surface of your soft tissue to slide over bone effortlessly. When pressure or friction is too great, excess fluid can build up in the bursa sac causing inflammation. When a bursa becomes inflamed, moving the affected area becomes very painful and movement can be difficult. Any actions that put pressure on the inflamed bursa can increase irritation and cause further inflammation and pain.
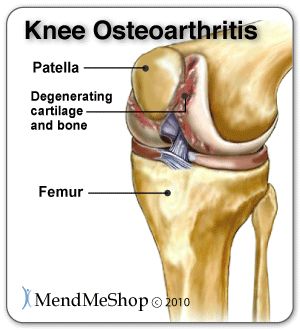
Arthritis is a condition that can affect the tissue lining in joints (this lining is called the 'synovium'). You may suffer from rheumatoid arthritis (RA) which is an autoimmune disease, or osteoarthritis (OA) which is a degenerative condition from wear and tear. When experiencing arthritis in general, inflammation from arthritis causes redness, heat, pain and swelling. Symptoms start with feeling pain and stiffness in the joint, reduced joint mobility, and swelling. It's possible for arthritis to cause tendonitis, with severe swelling in the joint arthritis can cause weakening in tendon tissue resulting in a strain or rupture.
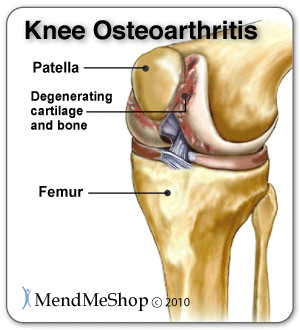
Patellor femoral arthritis causes pain in the front of your knee and can make it difficult to kneel or climb stairs. The kneecap slides up and down in a groove on the end of the thigh bone (trochlear groove). Patellofemoral arthritis occurs when the cartilage along the trochlear groove and on the underside of the patella wears down and becomes inflamed.
Muscle strain are known as a 'pulled muscle', this overstretching the tissue beyond its capacity. Athletes are at more of risk of muscle strains as they use their muscles everyday. Less inactive people also are at risk as their muscles become weak and over using them can strain the tissue. This 'pull' of the muscle fibers is micro-tears and even separation from the tendon. Pain and inflammation in the muscles, you may feel more muscle weakness, swelling, bruising or even pain when move your knee.
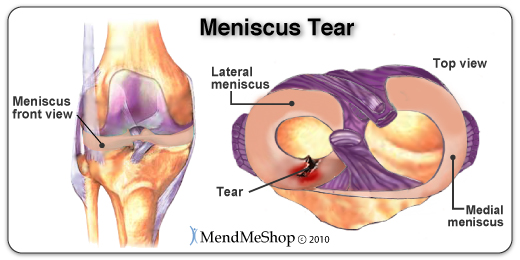
The meniscus is a rubbery, C-shaped disc that cushions your knee. Each knee has two menisci (plural of meniscus)-one at the outer edge of the knee and one at the inner edge. The menisci keep your knee steady by balancing your weight across the knee. A torn meniscus can prevent your knee from working correctly and pain and slight swelling are often the only symptoms.
Sprains happen to ligaments. Ligaments are fibrous tissue that connect bone to bone in the knee joint such as the ACL, PCL, LCL, or MCL. To much force on the joint pulls on the bones and overstretches the ligament tissue, causing micro-tears in ligament fibers. If the sprain is traumatic, the ligament may rupture under the force and surgery is required to completely recover. Anyone is at risk of for a ligament sprain, there are some that are at high risk, athletes in collision sports, football or ruby. Sometimes less impact can cause a slight sprain with the knee twisting inwards such as standing up for a chair. Pain and inflammation in the ligament affected, swelling, or even pain when move your knee.
Weakness in the knee as if it is unstable while walking up or down stairs or slopes. Pain with the extension of the knee, as well as may hearing a cracking noises when flexing and straightening your knee. Known as "pathological synovial plica syndrome" considered a embryonic relic. At the 12th week of life the synovial plica forms in the knee, as we grown and mature this tissue then is becomes entangled within the knee and is unable to dissolve and remains in our adulthood. Estimated that 50% of the population has the 'plicae' after birth. It is common for this condition to be over looked by doctors. (source: National Library of Medicine)
Usually seen in people over the age of 40 as the tissue as part of aging degenerates. A sudden trauma to the tendon may cause it to tear or may spontaneously tear with people suffering from diabetes mellitus, gout, systemic lupus erythematosus, rheumatoid arthritis, end-stage renal disease, prolonged systemic steroid use or hyperparathyroidism. Early surgical repair within 27hrs is the key to successful healing of the tendon. (source: National Library of Medicine)
If you are suffering from a complete rupture of the quadriceps tendon you will have a very painful and swollen knee. The rupture has left you unable to walk or you may walk with assistance or holding your leg as straight as possible. You may notice a gap in the tendon just above the kneecap where the muscle and tendon have broken away from the bone. Early surgical repair within 27hrs is the key to successful healing of the tendon. (source: National Library of Medicine)
A chemical reaction in the body, after injury to the soft tissue, the body is healing but instead of healthy tissue, it creates calcium in the tendon. If you are suffering calcific tendinitis of the quadriceps tendon, you may have pain and stiffness that may last for a few weeks to two months and suddenly disappear. If calcific tendinitis is return a number of times is now chronic you may notice your pain linger for a few months to years.
Causes a dull, aching pain in the front of your knee. There is damage or softening of the cartilage on the underside of the knee cap. Pain while walking up or down stairs, kneeling or squatting or after sitting for long periods of time with your knee bent.
Pain, inflammation, and swelling at the front of the knee cap and along the sides of the patellar tendon. Increased pain when standing for long periods of time, squatting or using stairs and or pain when you extended you knee. Hoffa's syndrome is caused by at pad either suffers a contusion or an injury, resulting in damage and swelling. This can lead to the Hoffa's pad becoming trapped between the femur and the patella every time the leg is extended.
Pain on the sides and around the knee cap. The kneecap slides up and down in a groove on the end of the thigh bone (trochlear groove). In some people the kneecap is pulled toward the outside of the knee and the kneecap does not slide in its groove. This condition normally affect adolescents and younger children.
Ligament tears, primarily of the anterior cruciate ligament (ACL), are commonly the season ending injuries we hear about in sports. Although male athletes make the headlines, women experience ACL tears 7-8 times more frequently than men due to hormonal and anatomical reasons.
The knee has 2 collateral (parallel) ligaments and 2 cruciate (crossing) ligaments. The medial collateral ligament (MCL) and the lateral collateral ligament (LCL) provide support to the knee by limiting the sideways motion of the joint. The anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL) stabilize the knee by limiting the rotation and the forward and backward movement of the joint.
Of the 2 collateral ligaments, the MCL is the one that is injured most often. This injury is often a result of a blow to the outer side of the knee.
Of the 2 cruciate ligaments, the ACL is the one that is injured most often. This injury occurs when the knee is locked with the foot planted and the knee is twisted quickly. Athletes required to make sudden directional changes or to slow down quickly and those in contact sports are at high risk for ACL tears, especially if they are wearing cleats or skis.
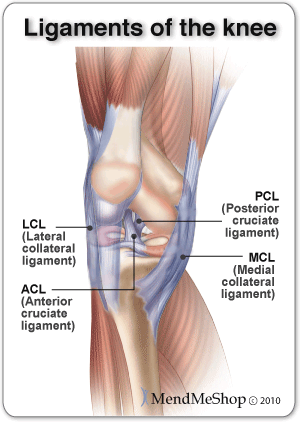
Minor tears may go unnoticed immediately and will appear a few hours later with pain and swelling. More serious ACL tears are accompanied by severe pain and often a popping sound. The knee may feel as though something has snapped and walking or bending the knee is usually impossible.
Administering ice and compression immediately will help reduce pain and swelling. Treatment differs depending on the degree of instability and the patient's activity level. Many ligament injuries heal with rest and home conservative treatments such as cold and heat (once swelling is down) . Circulatory Boost is exactly what the Knee TShellz Wraps® is made for.
Once your knee has improved somewhat, it is recommended that you build muscle strength around the knee with gentle stretching under the guidance of a physical therapist or physician to complete your return to normal and help prevent re-injury in the knee. If an injured ligament does not strengthen appropriately or an athlete continues to experience the knee giving way, arthroscopic surgery and ligament reconstruction may be necessary. For more information on ligament tears, click here.
The meniscus is a C-shaped piece of cartilage that works as a cushion between the femur and the tibia. Tearing of the meniscus occurs when the knee is twisted forcibly while under weight. As the body ages, cartilage deteriorates - this makes knee joints more susceptible to meniscal tears with minor movement. When the meniscus is torn, it starts to move abnormally inside the joint and it may become caught between the tibia and femur.
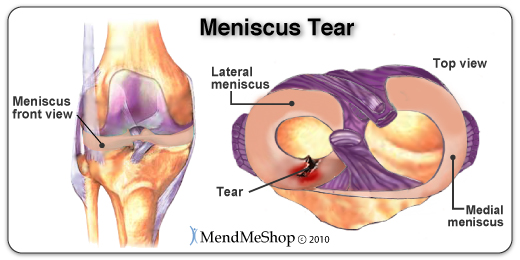
Those suffering from a meniscal tear commonly experience swelling, pain and difficulty moving the knee.
A minor tear in the meniscus may only require rest, a change in activity, and strengthening exercises to support the joint. Unfortunately, meniscal tears can be difficult to heal because blood supply is often limited to the outside edge of the meniscus cartilage. Circulation Boost will help prevent scar tissue accumulation and speed up healing by increasing the flow of blood and nutrients to the area. In the case of a large or complex tear or if disabling symptoms remain after 2-3 months, arthroscopic surgery may be recommended. For more information on meniscus function and tears, click here. (goes to mendmyknee.com)
Patellar Chondromalacia occurs when the cartilage enabling the femur and kneecap to glide smoothly over one another becomes damaged. This damage is caused by regular wear and tear or by repetitive trauma due to the knee muscles weakening and the patella (kneecap) becoming misaligned. Patellar Chondromalacia is very common in runners and is often termed as 'Runners Knee'.
Patellar Chondromalacia patients complain of tenderness under or around the kneecap and the pain often increases when using stairs or getting out of a chair. A grinding feeling may also occur when trying to straighten the knee.
When the injury becomes inflamed, icing is recommended and anti-inflammatory drugs may be prescribed. Strengthening the muscles around the knee joint, particularly the inner quadriceps is the best treatment to realign the patella. To prevent further damage to the cartilage, minimize impact exercises until the muscle strength increases. For more information on Patellar Chondromalacia, click here. (mendmyknee.com)
Bursitis occurs when the bursae swell from chronic irritation, inflammation and the accumulation of excess fluid within the bursa sacs. This is commonly caused by frequent kneeling and is referred to as "housemaid's knee" as it is often suffered by people whose work requires kneeling for extended periods of time.
Symptoms include knee pain and limited motion, along with swelling and redness over the kneecap. When walking, sufferers experience extreme pain and stiffness that worsens when using stairs. A patient may also experience a fever if the bursae become infected.
When inflammation and pain occur, it is recommended that any aggravating activity be discontinued. However, even daily activities can inflame the tender sacs and cause healing time to be extended. RICE will help to ease the symptoms and promote healing. In severe cases, draining the bursae may be necessary and if fluid accumulation continues, removing the bursa may be the consequence. For more information on prepatellar bursitis, click here. For more information on pes anserine bursitis, click here. (both links go to aidmybursa.com)
A fracture of the patella, can occur from an impact on the kneecap; such as in the case of a car accident, a fall or contact while playing a sport. A fractured patella causes pain and tenderness, swelling, a limited range of motion and the inability to walk. Symptoms may also include muscle spasms and grating of bone if fragments are loose in the joint.
If the fractured bones are lined up, surgery is not necessary and a leg cast is used to immobilize the leg allowing the bones to heal. If the bones are not aligned, surgery is required and the fractured ends are set and held in place with pins and wires.
The patellar tendon joins the kneecap to the shin bone and works as part of the extensor mechanism allowing the knee to straighten out. Patellar tendonitis is an injury caused by overuse or recurring trauma to the tendon and is often seen in athletes of jumping sports like basketball or volleyball.
Sufferers experience pain and swelling at the front of the knee along with a limited range of motion. The pain often becomes more severe with jumping or kneeling.
Treatment begins with resting the knee and avoiding the symptom causing activity until symptoms settle. Cold compression and anti-inflammatory medication will assist in controlling the inflammation, decreasing swelling and managing pain. Once the tendon is no longer inflamed, PT sessions, hamstring stretching and limiting high impact activities is recommended. For more information about patellar tendonitis, click here.
Osteoarthritis is caused by the cartilage in the knee deteriorating with wear and tear or because of trauma to the joint, ultimately leaving only bare bone. It is the most common type of knee arthritis and is also called degenerative joint disease or wear-and-tear arthritis. The risk of osteoarthritis increases with age and for people who are genetically predisposed to the disease, are overweight or have suffered knee trauma chances are even greater.
Although osteoarthritis worsens with time, sufferers experience periods of flare-ups and remission. Symptoms include increased pain with use throughout the day, joint stiffness, swelling, and tenderness. Patients often experience grinding, clicking, locking or feelings that the knee may give out. Movement of the joint can be limited and deformity may occur over time as bones become damaged.
Pain may be managed and damage minimized by decreasing the burden on the knee joint with weight loss or use of a walking aid. Low-impact and aquatic exercises and PT will strengthen the muscles to support the knee joint.
Cold compression wraps, anti-inflammatory medications, and anti-inflammatory injections can reduce pain and inflammation. As discussed early, a recent study has called into question the benefit of arthroscopic surgery and you should discuss your options with a physician before making any decisions about surgery.
If osteoarthritis pain cannot be managed by these methods, surgical options may be considered; knee arthroscopy, tibial osteotomy or knee replacement surgery, depending on your injury. For more information on knee osteoarthritis, click here (mendmyknee.com) and follow the links on the left.
Osgood-Schlatter ("oz-good shlot-ter"") is a disease experienced by adolescents, usually athletes, during a period of rapid growth. It occurs when the patellar and/or tendon pulls away from the tibia and becomes inflamed. This inflammation is a result of excess strain on the tendon due to muscles and bones growing at varying rates.
Osgood-Schlatter Disease causes swelling and pain below the knee, just above the tibia. The pain increases with exercise and is relieved when the knee is at rest. It is also common to experience tightening of the muscles and limping after strenuous activity.
As the growth spurt ends, muscles and bones catch up with one another, the patellar tendon strengthens and pain and swelling subsides. In the meantime, resting the tendon is the best way to treat Osgood-Schlatter Disease. If the pain is mild some activity may be continued, but severe pain requires discontinuation of the sport. Pain medication, heating the joint before playing and icing it afterwards can control swelling and pain. It is important to not play through the pain and attend to the injury as needed or recovery time is extended.
A patellar (kneecap) dislocation occurs when one of the ligaments securing the patella to the knee, usually the medial patellofemoral ligament (MPFL), tears and allows the patella to fall out of its groove.
The most obvious symptom is the kneecap's ability to move freely from side to side. In addition, intense pain, swelling and the inability to walk or straighten the knee will be experienced.
Bracing the knee to allow the MPFL to heal is the first treatment option. However, this can be ineffective as it is difficult for the MPFL to heal without proper tension. If the ligament does not heal correctly, the chance of dislocation recurring is high. Surgery to repair the ligament may be necessary and should be discussed with a physician if proper healing does not occur.
Gout is a type of arthritis that is identified by a severe and rapid onset of pain. The pain is a result of an accumulation of uric acid in the knee. It is often an inherited disease but other factors contributing to gout include obesity, excessive alcohol consumption, kidney malfunctions and certain types of cancer.
Gout sufferers will experience sudden and severe pain, warmth, redness, swelling and tenderness of the knee joint. They may also suffer from kidney stones or kidney failure which causes the uric acid to enter the blood stream.
Preventing gout attacks can be achieved with weight reduction, limited alcohol consumption and adequate fluid consumption. Lowering uric-acid levels with medication or dietary modifications (i.e. limiting purine-rich foods and increased consumption of dairy products) can also reduce inflammation. When gout attacks occur, anti-inflammatory medications may be used to control the pain. Other medications available to gout sufferers include colchicines, which is used to reduce gout pain quickly, and other otc meds used to prevent future attacks. As with any medication, it is important to consult your doctor to see if the medication is right for you.
Taking measures to protect your knees and maintain healthy joints is something everyone can do to prevent knee pain. Should knee injury or disease become a part of your life, understanding your condition is the first step in determining the appropriate treatment. Get an accurate diagnosis from your physician and discuss your options. Proper treatment will allow you to resume your activities faster and safer.
Product Advisors are available 9:00 am to 5:00 pm Eastern Standard Time Monday to Friday.
I want to learn more about Post-Surgery Recovery
I want to learn more about TShellz Wrap® Circulatory Boost
I want to learn more about Ice & Heat: Which Is Better For Treatment?
I want to learn more about Tendonitis Treatments
I want to learn more about Tendonitis Surgery
During your recovery, you will probably have to modify and/or eliminate any activities that cause pain or discomfort at the location of your soft tissue injury until the pain and inflammation settle. The more diligent you are with your treatment and rehabilitation, the faster you will see successful results!
Please be aware that this information is neither intended nor implied to be a substitute for professional medical advice. CALL YOUR HEALTHCARE PROVIDER IMMEDIATELY IF YOU THINK YOU MAY HAVE A MEDICAL EMERGENCY. Always seek the advice of your physician or other qualified health provider before using any of our outstanding products to make sure they are right for you and your condition or if you have any questions regarding a medical condition. Always see your doctor for a proper diagnosis as there are often many injuries and conditions (some very serious) that could be the cause of your pain.
© 2025 In.Genu Design Group, Inc. Contact Us